For multiple decades, Kay was a physiotherapist working with those with multiskeletal conditions. This involved direct outpatient referrals from GPs where she would provide treatment through face-to-face appointments. Kay also worked on the orthopaedic pathway. In March, Covid-19 changed her job forever.
By George Willoughby
“I often say to people it is like I am trying to do physiotherapy with my hands tied around my back and blindfolded when I am on the phone to somebody. It is really difficult but you find a way to get used to it.”
When the pandemic hit, Kay and the rest of the team were redeployed to try and create capacity in hospitals in preparation for Covid-19 patients. The concern was that hospitals would not be able to manage the influx of Coronavirus patients. Consequently, outpatient departments - such as physiotherapy - were closed.
This was a national effort and the impact on current patients and staff was significant.
“We were redeployed to an unused nursing home. It was used as an overflow from the hospital and at the start of the pandemic, the idea was to empty the hospitals ready for Covid-19 patients.
“In the nursing home, we were acting as a discharge to assess unit. So anybody that had received treatment in hospital would be transferred into the care home. We would assess these patients and work out where they would move to next.
“As a result of this, the outpatient physiotherapy department closed. We could not see any patients because all of the staff were sent to different units. We were being asked to do a completely different job to what we had been doing all of our careers. It was quite a shock.”
Outpatient departments across England have shut meaning the number of appointments has fallen significantly.
Changes to the profession
The nature of physiotherapy work has changed because of the fluid nature of the pandemic. Preparing for such a rapid alteration is extremely difficult.
“For those of us who have been redeployed. The change is massive. It is a completely different job,” - said Kay.
A large part of why the job is so different now and why it will continue to be is because most face-to-face appointments have stopped.
This has consequences for the wellbeing of patients, but it also has posed teething problems for Kay and her colleagues.
“Before the pandemic, people would have a 40-minute face-to-face appointment. We would often follow those people up maybe four to six times and give people exercises to do and support them in their exercise therapy. There would be a mixture of sessions.
“We are now doing these assessments on the phone rather than seeing people face-to-face and talking about their problem,” says Kay. “We talk to people via a video link, send out exercise sheets in emails whereas before we would be able to meet the person and give them support.”
The switch to online consultations was one of the biggest challenges Kay spoke of. Not only was she trying to become accustomed to a new way of working, so were her patients.
People who need physiotherapy vary in age group, so for some of her patients, online telephone and video calls were a relative success.
However, not everyone is going to have the same technological capabilities.
“If the person has not used a camera then it is difficult. You end up phoning them. You cannot see their posture, what movement they have in their joints and of course, we cannot do the full physical tests. It just is not anywhere near as good quality service.
“We have had quite a few issues in that the technology has not been good. Often with the sound system, you cannot hear people on the line or the video link will break down.”
Limitations of online consultations
Outpatient departments are having to incorporate online appointments into their services. For areas like physiotherapy, patients require bodily examinations and a rapport is built with the physio.
Telephone and video appointments do not have the same effect compared to meeting face-to-face. Kay was quite open about this saying that “things could be missed when it is over the phone.”
“You do not feel like you have been assessed properly. For whatever reason, you have not made a proper connection with the patient,” - said Kay.
“Things could be missed. We try and describe certain tests to people, but we cannot see if they are doing them properly. I cannot possibly know. The assessment is flawed.”
The new discharge to assess units that Kay spoke about were something the health service was planning to implement shortly. Covid-19 has accelerated plans, so the changes to physiotherapy treatment were going to happen regardless.
Over time, it may get easier. However, in Kay’s opinion, there will always be doubts over the effectiveness.
“If the person on the other end of the line has the camera set up well and can listen to my instructions, it can be very successful. We have become more savvy and skilled at using instructions over the phone, rather than relying on our eyes. We are learning on the job really, but one day we will get it right.”
England recently came out of a second national lockdown. The latest figures from NHS Digital show that there were one million fewer outpatient appointments attended in September 2020 compared to the same point last year.
Certain treatment types also require different approaches. Physiotherapy is just one department that is dealing with a paradigm shift in the way appointments are carried out.
Digital future
Prime Minister Boris Johnson announced that restrictions in England are expected to stay in place until the Spring.
Kay wants to try and embrace technology and proposes a revised system following confirmation of the Covid alert level announcement.
“I do not think we need to completely throw it out of the water because I think there are some benefits. It is more convenient for lots of people who can pick up the phone on their way to work and they have some advice on the end of the line.
“But, there needs to be a safety net to make sure the assessment is correct. I suppose one way of doing it would be that you start giving initial advice. If that works, great, if it does not go further down the line and have a face-to-face appointment.
“There are uses with the new development, but there are also problems that need to be ironed out. You have got to have face-to-face as well as the technology to make it work.”
The social side to physiotherapy
Ultimately, the Covid-19 pandemic has changed the way outpatient appointments will be delivered.
Telephone and video calls are alternative methods that patients and staff have been adapting to.
Kay mentioned some advantages including shorter waiting times and fewer unnecessary appointments.
However, something that can get overlooked with physiotherapy is social interaction. This can be with the physio themselves but also others who attend sessions.
“The social side is therapy for some people. If you take that away, you are removing a lot of the therapy. Socialising is often part of the treatment.
“Pre-pandemic we used to run classes. Part of the reason we ran classes was to allow interaction with people who had the same condition. There is no way we can run those and the benefits are lost when we have moved online.
“Physiotherapy is not just about exercise. The nuance of physio is encouraging social interaction and this is to help them mentally too.”
Looking ahead to the future, it is clear that outpatients requiring physiotherapy will have a different kind of service compared to pre-Covid-19.
The challenge is whether departments can host classes again and also spend time with patients individually.
Combining phone calls and face-to-face appointments seems to be the approach for physiotherapy services.
“I can see it being useful to integrate technology into our system, only if we do it right.”
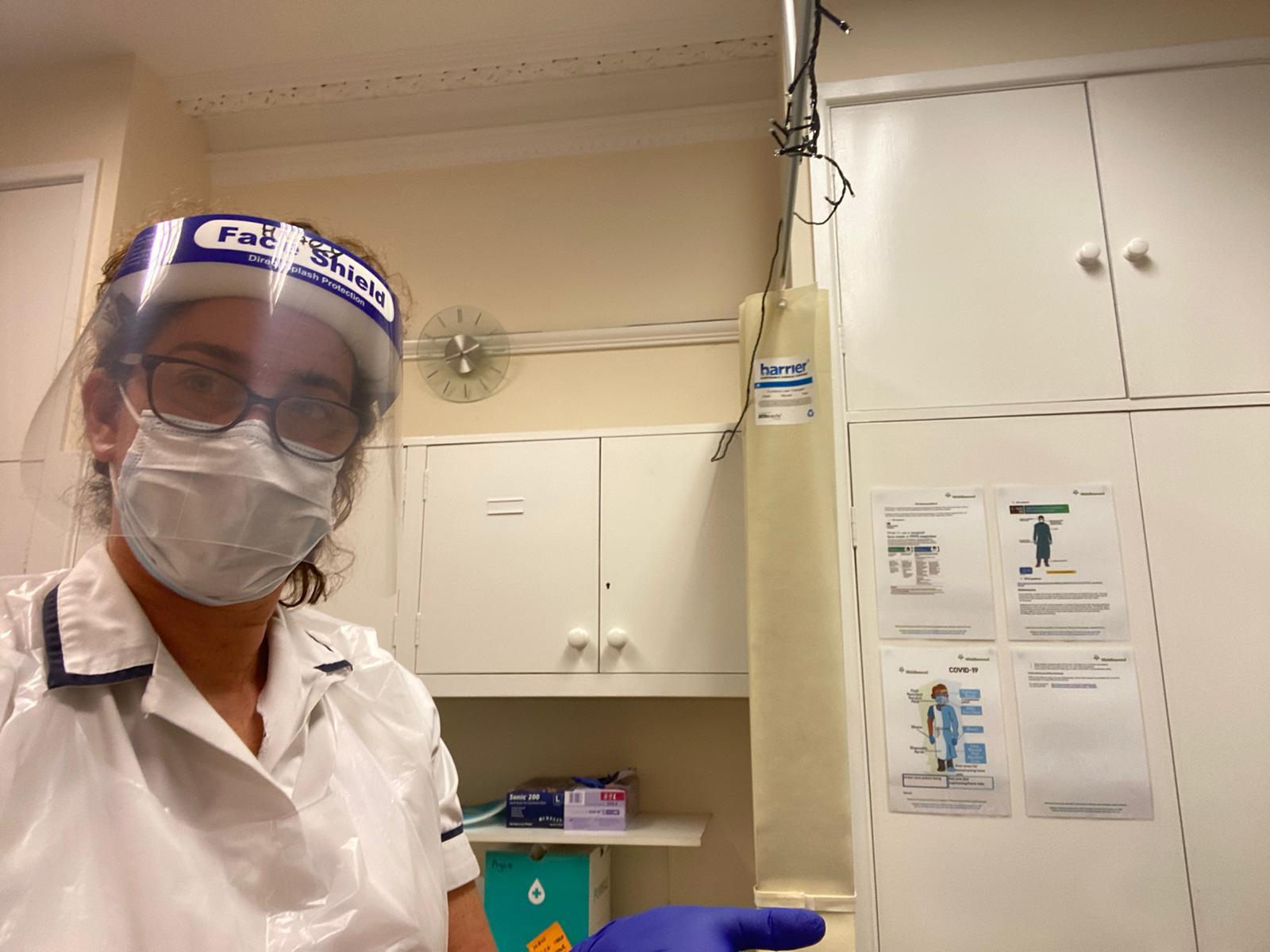
Picture Source: Kay Hebden